Semen testing after a vasectomy or during fertility checks sounds straightforward, but every year, nearly 48 percent of men skip submitting their post-vasectomy semen samples. Most people assume once the procedure is over, everything is settled. Here is the twist. Skipping these crucial tests can leave you unknowingly fertile, showing that the biggest risk in male reproductive health might be silence, not science.
Table of Contents
- Common Problems In Semen Sample Collection
- How Testing Errors Affect Vasectomy Confirmation
- Solutions To Improve Accuracy And Reliability
- When To Retest And Seek Advice
Quick Summary
| Takeaway | Explanation |
|---|---|
| Proper Sample Collection is Crucial | Ensuring optimal conditions during semen sample collection, including temperature control and avoiding contaminants, is vital for accurate test results. |
| Follow Testing Protocols Thoroughly | Noncompliance in submitting semen samples post-vasectomy can lead to undetected fertility; following recommended testing timelines and protocols is essential. |
| Recognize When to Retest | Awareness of specific indicators, such as the presence of motile sperm beyond established timelines, necessitates professional consultation for potential surgical issues. |
| Leverage Technological Advancements | Utilizing innovative tools like smartphone-based semen analyzers can enhance testing accuracy and accessibility for home-based monitoring and analysis. |
| Patient Education is Key | Understanding the testing process, including sample collection and transportation, significantly improves compliance and accuracy in semen assessments. |
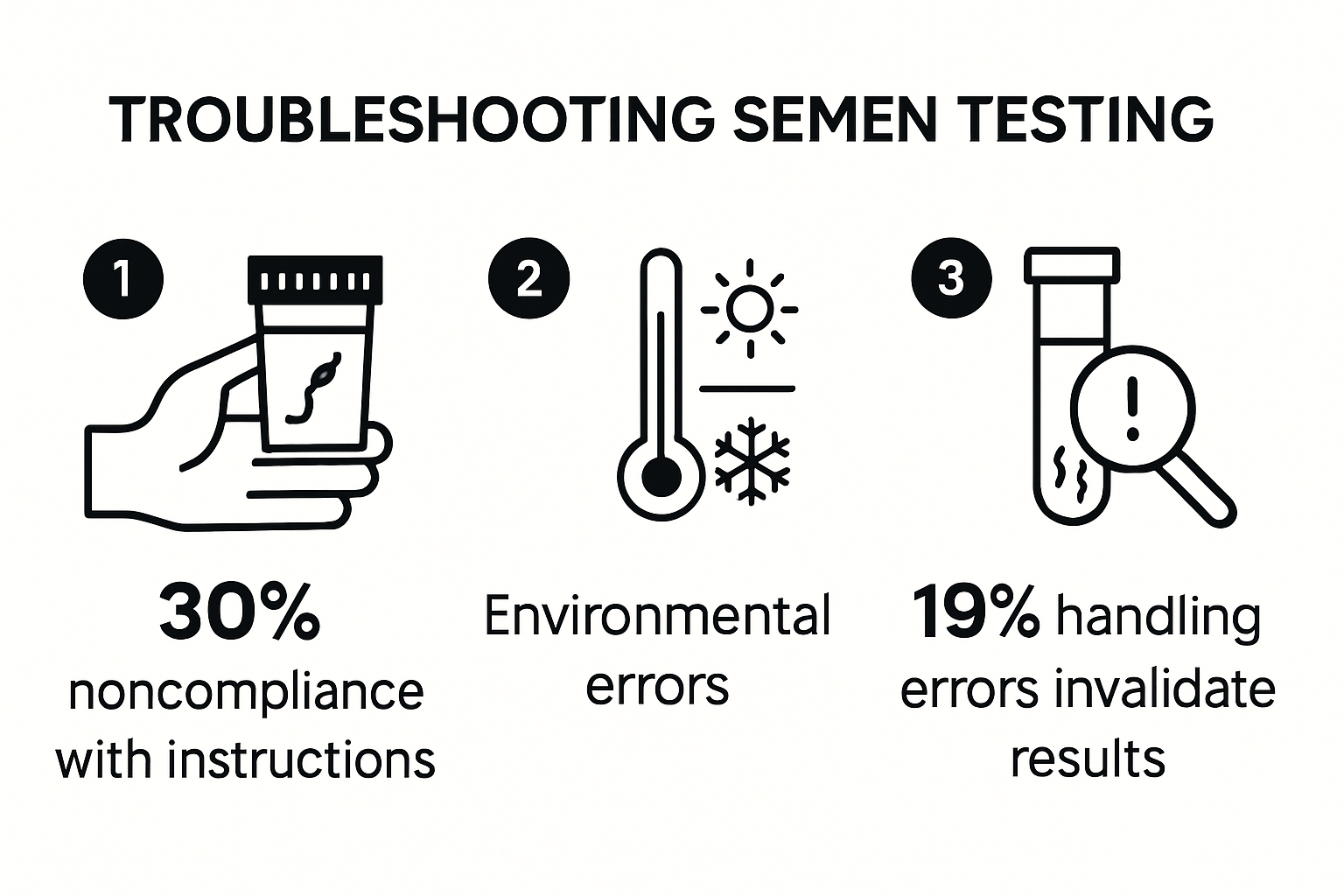
Common Problems in Semen Sample Collection
Successful semen testing requires precision and careful attention to detail. Men undergoing vasectomy confirmation or fertility assessment often encounter challenges that can compromise sample quality and test results. Understanding these potential issues is crucial for obtaining accurate diagnostic information.
Collection Environment and Technique Challenges
Collecting a semen sample involves more complexity than many individuals realize. Learn more about optimal sample collection techniques to ensure reliable results. Environmental factors play a significant role in sample integrity. Temperature sensitivity, contamination risks, and timing are critical elements that can dramatically impact test outcomes.
According to research from the National Institutes of Health, inappropriate sample collection can lead to misleading fertility assessments. Common mistakes include using incorrect collection methods, exposing the sample to extreme temperatures, or introducing contaminants that compromise sperm viability.

Lubrication and Sample Handling Errors
One of the most frequent troubleshooting semen testing issues involves lubrication and handling techniques. Clinical research demonstrates that using inappropriate lubricants can severely damage sperm quality. Substances like Vaseline, standard personal lubricants, water, or saliva can destroy sperm motility and reduce overall sample effectiveness.
Proper sample transport is equally critical. Semen samples must be maintained at a consistent temperature between 20°C to 37°C and delivered to the laboratory within one hour of collection. Delays or temperature fluctuations can cause significant degradation of sperm cells, rendering the test results unreliable.
Psychological and Practical Collection Barriers
Beyond technical challenges, psychological factors can significantly impact semen sample collection. Anxiety, performance pressure, and discomfort with the collection process often lead to suboptimal samples. Many men struggle with the clinical nature of semen collection, which can create stress that indirectly affects sample quality.
To mitigate these challenges, experts recommend creating a comfortable, private collection environment. Using at-home testing kits can help reduce psychological barriers by providing a more relaxed and familiar setting. Proper preparation, following detailed instructions, and maintaining a calm approach are essential for obtaining an accurate semen sample.
By understanding these common problems in semen sample collection, individuals can take proactive steps to ensure the most reliable testing experience. Careful attention to technique, environment, and personal comfort can dramatically improve the accuracy of vasectomy confirmation and fertility assessments.
To help visualize common challenges faced during semen sample collection and the impact on test accuracy, the following table summarizes key collection problems and their possible consequences:
| Problem Area | Example Issues | Potential Impact on Results |
|---|---|---|
| Environment & Technique | Extreme temperature, contamination, incorrect methods | Misleading fertility assessment, inaccurate counts |
| Lubrication & Handling | Use of Vaseline, standard lubricants, water, saliva | Destroyed sperm motility, poor sample effectiveness |
| Transport Timing & Temperature | Delayed delivery, temperature fluctuation | Sperm degradation, unreliable test results |
| Psychological & Practical Barriers | Anxiety, discomfort, unfamiliar setting | Suboptimal samples, increased collection failures |
How Testing Errors Affect Vasectomy Confirmation
Vasectomy confirmation requires precision and thorough testing to ensure male sterilization. Testing errors can significantly compromise the reliability of results, potentially leading to unexpected fertility risks or unnecessary additional procedures.
Noncompliance and Incomplete Testing Protocols
Discover the nuances of vasectomy testing accuracy to understand potential pitfalls. A critical challenge in vasectomy confirmation involves patient noncompliance and incomplete testing. Research published in the Journal of Urology revealed a startling statistic: nearly 48% of vasectomy patients did not submit any postoperative semen samples, dramatically increasing the risk of undetected fertility.
These testing gaps create significant uncertainties. Without consistent and comprehensive semen analysis, patients may mistakenly believe they are sterile when viable sperm could still be present. The absence of rigorous follow-up testing represents a substantial risk for unintended pregnancy.
Persistent Sperm Detection Complications
Advanced microscopic techniques have exposed complex challenges in determining complete sterility. Research from the National Institutes of Health indicates that rare non-motile sperm (RNMS) can persist in semen samples for over a year after vasectomy. This unexpected finding complicates traditional sterility confirmation methods.
The British guidelines for post-vasectomy semen analysis now require two centrifuged semen samples showing RNMS to grant definitive clearance. This stringent protocol has increased RNMS detection from 18% to 27%, demonstrating the intricate nature of verifying complete sterility.
Technological and Procedural Limitations
Testing errors emerge from multiple sources beyond patient compliance. Microscopic analysis techniques, sample handling procedures, and laboratory protocols all contribute to potential inaccuracies. Variations in centrifugation methods, microscope calibration, and technician expertise can introduce subtle but significant variations in sperm count and motility assessments.
Modern at-home testing approaches aim to standardize these processes, reducing human error and providing more consistent results. By implementing strict quality control measures and utilizing advanced detection technologies, these methods seek to minimize the uncertainties inherent in traditional testing protocols.
Understanding these testing complexities is crucial for individuals seeking definitive vasectomy confirmation. Patients must remain proactive, follow comprehensive testing guidelines, and work closely with healthcare professionals to ensure accurate results. The journey to confirmed sterility requires patience, precision, and a thorough understanding of potential testing limitations.
Here is a table summarizing how testing errors or limitations at different stages can affect vasectomy confirmation results:
| Error or Limitation | Description | Risk/Impact |
|---|---|---|
| Noncompliance with Testing | Patient does not submit sample post-vasectomy | Undetected ongoing fertility, pregnancy risk |
| Persistent Rare Non-Motile Sperm (RNMS) | RNMS detected over a year after vasectomy | Delayed sterility confirmation, repeat tests |
| Microscopy/Procedural Variations | Differences in technique, calibration, centrifugation | Inconsistent sperm detection/counts |
| Sample Handling Errors | Improper sample collection, contamination, transport delays | Unreliable or false-negative results |
Solutions to Improve Accuracy and Reliability
Addressing the challenges in semen testing requires innovative approaches and technological advancements. Researchers and medical professionals are continuously developing solutions to enhance the accuracy and reliability of vasectomy confirmation and fertility assessments.
Advanced Technological Interventions
Explore cutting-edge semen analysis techniques that are revolutionizing diagnostic accuracy. Computer-Aided Sperm Analysis (CASA) systems represent a significant breakthrough in improving testing precision. Research published in advanced medical journals demonstrates that these sophisticated technologies can dramatically reduce human subjectivity and error in sperm evaluation.
Smartphone-based semen analyzers are emerging as a game-changing solution. Scientific studies indicate these portable devices can reliably assess sperm concentration and motility, providing unprecedented accessibility for home-based monitoring. This technological innovation bridges the gap between clinical precision and patient convenience.
Standardized Testing Protocols
Consistent and structured testing protocols are crucial for reliable results. Clinical guidelines from urological experts recommend conducting the first post-vasectomy semen analysis (PVSA) between 6 and 16 weeks after the procedure. This specific timing window ensures the most accurate assessment of vasectomy success.
Key recommendations include:
- Performing multiple semen analyses to confirm sterility
- Using centrifugation techniques to detect rare non-motile sperm
- Implementing strict quality control measures in sample processing
Patient Education and Engagement
Improving testing accuracy extends beyond technological solutions. Patient education plays a critical role in ensuring reliable results. Men must understand the importance of:
- Following precise sample collection instructions
- Completing recommended follow-up testing
- Maintaining proper sample transportation conditions
At-home testing kits have emerged as a powerful tool in addressing patient compliance. By providing comprehensive instructions, user-friendly interfaces, and secure result reporting, these solutions reduce the psychological barriers that often prevent thorough testing.
The future of semen testing lies in a holistic approach that combines advanced technology, standardized protocols, and patient-centered design. By addressing the multifaceted challenges in vasectomy confirmation and fertility assessment, healthcare providers can offer more reliable, accessible, and precise diagnostic solutions.
Continued research and technological innovation will be essential in refining these approaches, ultimately providing men with more confidence in their reproductive health assessments.
When to Retest and Seek Advice
Navigating post-vasectomy semen testing requires understanding precise timing and recognizing potential warning signs that demand professional consultation. Knowing when to retest and seek medical advice is crucial for confirming successful male sterilization and preventing unintended fertility complications.
Recommended Testing Timelines
Understand the critical windows for post-vasectomy testing to ensure accurate results. Clinical guidelines recommend conducting the first post-vasectomy semen analysis (PVSA) at least 12 weeks after surgery and following a minimum of 20 ejaculations. This specific timeframe allows sufficient healing and ensures a comprehensive assessment of surgical success.
Key testing milestones include:
- Initial test at 12 weeks post-procedure
- Follow-up tests if initial results show sperm presence
- Annual or biannual monitoring for patients with persistent rare non-motile sperm
Identifying Retest Indicators
Urological Association guidelines provide clear parameters for retesting. If motile sperm are detected six months post-vasectomy, a repeat vasectomy should be strongly considered, as this indicates potential surgical recanalization or procedural failure.
Additional retest scenarios include:
- Persistent non-motile sperm counts exceeding 100,000/mL beyond six months
- Inconsistent or inconclusive initial test results
- Significant changes in reproductive health or medical history
Professional Consultation Recommendations
Seeking professional medical advice becomes critical under specific circumstances. Patients should consult a urologist or reproductive health specialist if they experience:
- Continued presence of motile sperm after six months
- Unusual pain or complications following the vasectomy
- Concerns about potential fertility restoration
At-home testing provides an accessible first step, but it cannot replace comprehensive medical evaluation. Healthcare professionals can offer nuanced interpretations of test results, recommend additional diagnostic procedures, and provide personalized guidance based on individual medical histories.
The journey of post-vasectomy confirmation is not just about obtaining a single clear result but maintaining ongoing reproductive health awareness. By understanding testing protocols, recognizing potential complications, and proactively seeking professional advice, men can ensure the most accurate and reliable assessment of their reproductive status.
Remember, while at-home testing offers convenience and initial insights, it should be viewed as a complementary tool to professional medical care, not a complete replacement for expert consultation and comprehensive reproductive health management.
Frequently Asked Questions
What are common problems in semen sample collection?
Common issues include incorrect collection methods, contamination, and exposure to extreme temperatures, all of which can compromise sperm viability and test accuracy.
Why is it important to follow semen testing protocols post-vasectomy?
Following testing protocols is crucial because nearly 48% of men do not submit post-vasectomy samples, which can lead to undetected fertility and unintended pregnancies.
When should I retest after a vasectomy?
The first post-vasectomy semen analysis should ideally be conducted at least 12 weeks after the procedure, following at least 20 ejaculations.
How can I improve the accuracy of my semen test results?
Improving accuracy involves adhering to proper sample collection techniques, utilizing at-home testing kits for comfort, and understanding the importance of timely transportation to the laboratory.
Recommended
- Why Test Semen Sample: Answers for Vasectomy & Fertility 2025
- Why Semen Testing Is Critical: Insights for Men and Clinics
- Semen Analysis and Fertility Planning: Insights for Vasectomy and Conc
- Routine Semen Analysis Benefits for Vasectomy and Fertility 2025
- Top Challenges in Post Vasectomy Testing: 2025 Guide for Patients and
- Post Vasectomy Semen Test Timing - Understanding When





