Sperm health is not just a detail for would-be dads. It is a key player in fertility, and in 2025, the science has made it clearer than ever. Here is the shocker. A healthy sperm count should be at least 16 million sperm per milliliter. Most people think you only need a high number, but that is just the tip of the iceberg. Motility, shape, and even your lifestyle choices can make or break your chances, and new research is rewriting the rules.
Table of Contents
- How To Identify Signs Of Healthy Sperm
- Key Factors That Affect Sperm Health
- Healthy Sperm After A Vasectomy: What To Know
- Improving Sperm Health For Conception Success
Quick Summary
| Takeaway | Explanation |
|---|---|
| Sperm Concentration Affects Fertility | Healthy sperm concentration should be at least 16 million sperm per milliliter; below this can hinder conception efforts. |
| Diet Can Enhance Sperm Motility | Nutritional patterns like Mediterranean and DASH diets improve sperm movement, with at least 30% of sperm showing progressive motion being ideal. |
| Physical Activity Improves Sperm Quality | Regular moderate-intensity exercise supports better sperm quality and aids in weight management, which positively influences reproductive health. |
| Stress Management Is Crucial | Chronic stress negatively impacts hormone levels and sperm production; adopting stress reduction techniques can significantly benefit reproductive health. |
| Monitoring Post-Vasectomy Sperm Health Is Important | After a vasectomy, consistent monitoring through semen analysis is key to confirming sperm clearance and understanding long-term sperm health. |
How to Identify Signs of Healthy Sperm
Understanding the characteristics of healthy sperm is crucial for men assessing their reproductive health and fertility potential. Sperm quality involves multiple complex factors that go beyond simple quantity. Learn more about comprehensive sperm assessment to gain deeper insights into male reproductive wellness.
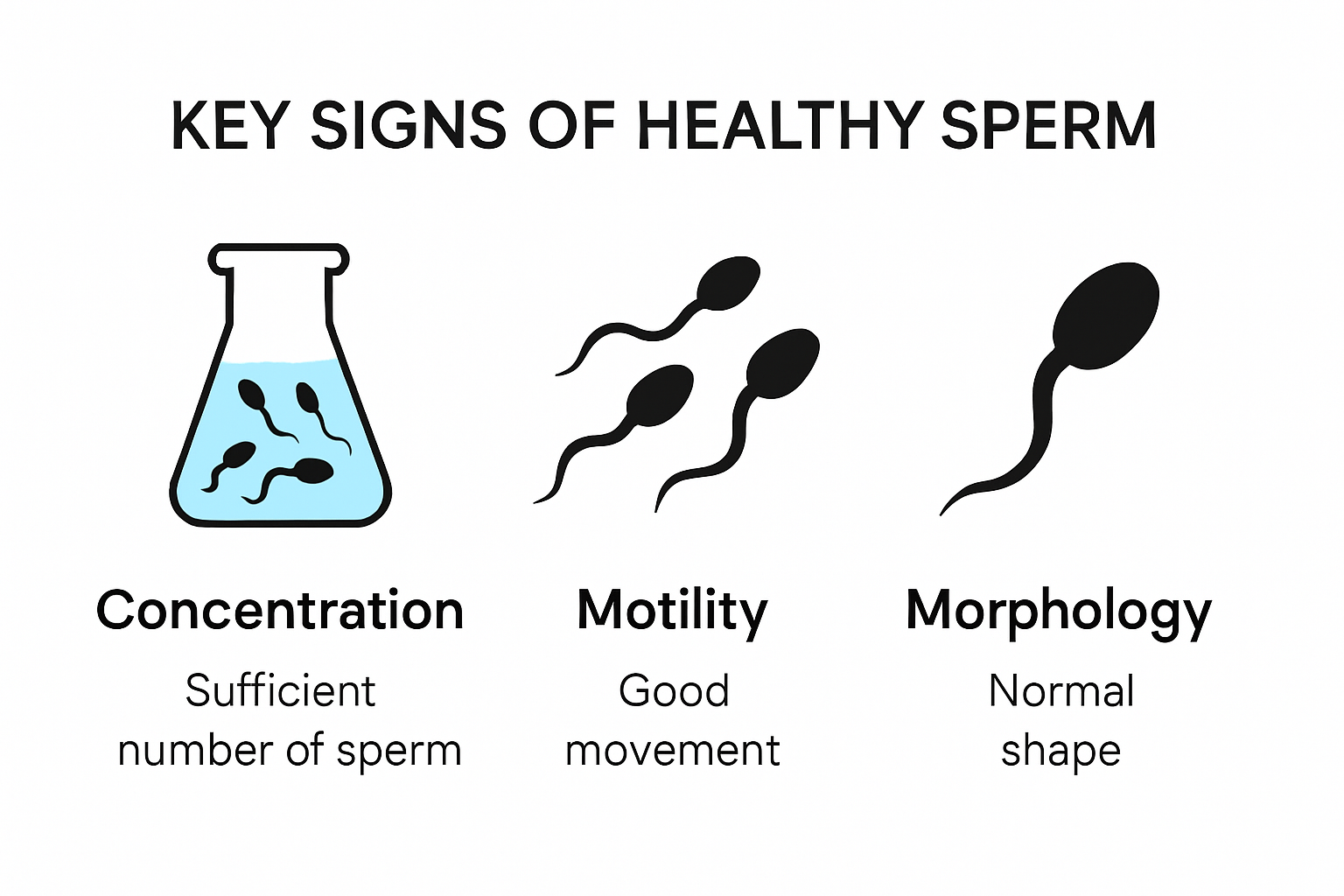
Sperm Concentration and Count
Sperm concentration represents the number of sperm cells present in a specific volume of semen. According to the World Health Organization, healthy sperm concentration should be at least 16 million sperm per milliliter. This metric is fundamental in determining male fertility potential. Men with concentrations below this threshold might experience challenges when trying to conceive.
Research from fertility specialists suggests that sperm count can fluctuate based on various lifestyle and environmental factors. Factors like stress, diet, exercise, and exposure to environmental toxins can significantly impact sperm concentration. Regular monitoring helps men understand their reproductive health trajectory.
Sperm Motility and Movement
Sperm motility refers to the ability of sperm to move effectively and progressively towards an egg. Scientific studies indicate that motility is more accurate in distinguishing fertile from infertile men compared to morphology. Healthy sperm should demonstrate progressive movement, with at least 30% of sperm showing forward motion.
Interestingly, nutrition research reveals that dietary patterns like Mediterranean and DASH diets are associated with improved sperm motility. Men can potentially enhance their sperm movement through strategic nutritional choices, emphasizing whole foods, lean proteins, and antioxidant-rich ingredients.

Sperm Morphology and Structure
Sperm morphology examines the physical shape and structure of sperm cells. According to reproductive health guidelines, normal morphology should exceed 4% of total sperm. Abnormal sperm shapes can indicate potential fertility challenges. These structural variations might impact the sperm’s ability to penetrate and fertilize an egg.
Advanced semen analysis techniques now allow men to comprehensively assess their sperm health from the comfort of their home. By understanding these key indicators, men can take proactive steps towards optimizing their reproductive potential and addressing any underlying concerns with medical professionals.
Remember that while these metrics provide valuable insights, individual fertility is complex. Consulting with a healthcare provider for personalized guidance remains the most reliable approach to understanding reproductive health.
To help summarize the main parameters of healthy sperm described above, the following table outlines optimal target values highlighted in the article.
| Sperm Quality Parameter | Healthy Target Value | Description |
|---|---|---|
| Sperm Concentration | ≥ 16 million/mL | Number of sperm per milliliter of semen |
| Motility | ≥ 30% with progressive movement | Proportion of sperm moving effectively towards the egg |
| Morphology | > 4% normal forms | Percentage of sperm with normal shape and structure |
Key Factors That Affect Sperm Health
Male reproductive health is influenced by a complex interplay of environmental, lifestyle, and physiological factors. Understanding these elements is crucial for maintaining optimal sperm quality and overall fertility. Explore our comprehensive guide to understanding sperm health dynamics.
Environmental and Lifestyle Impacts
Environmental exposure plays a significant role in sperm health. Research from environmental health experts reveals that air pollutants such as particulate matter (PM2.5 and PM10), sulfur dioxide (SO₂), and nitrogen dioxide (NO₂) can dramatically impact sperm quality. These pollutants are linked to decreased sperm motility and abnormal sperm morphology, highlighting the importance of environmental awareness.
Obesity emerges as another critical factor affecting male reproductive health. Scientific studies demonstrate that excess body weight correlates with reduced sperm concentration and compromised motility. The underlying mechanisms involve hormonal imbalances and increased oxidative stress, which can significantly impair sperm production and overall reproductive potential.
Substance Use and Hormonal Disruption
Substance consumption presents a substantial threat to sperm health. Chronic alcohol consumption research indicates that prolonged alcohol use can disrupt hormonal balance, leading to decreased testosterone levels and increased estrogen levels. This hormonal imbalance directly impacts sperm production, quality, and reproductive capabilities.
Tobacco and recreational drug use similarly pose significant risks. Smoking has been consistently linked to reduced sperm count, decreased motility, and increased DNA fragmentation. Marijuana use can lower testosterone levels and impair sperm production, potentially leading to long-term fertility challenges.
Nutritional and Stress Considerations
Nutritional status plays a pivotal role in maintaining optimal sperm health. Deficiencies in key nutrients like zinc, selenium, vitamin D, and antioxidants can compromise sperm quality. Nutrition experts recommend diets rich in whole foods, lean proteins, and antioxidants to support reproductive health.
Chromic stress emerges as another significant factor. Elevated stress levels trigger hormonal cascades that can negatively impact sperm production. The release of cortisol and other stress hormones can suppress testosterone production and reduce overall sperm quality. Advanced semen analysis techniques now enable men to track these subtle changes and take proactive steps toward improving their reproductive health.
Understanding these factors empowers men to make informed lifestyle choices. While individual experiences may vary, adopting a holistic approach to health can significantly improve sperm quality and overall reproductive potential. Regular medical consultations and comprehensive health assessments remain the most reliable method for monitoring and maintaining optimal sperm health.
Below is a summary table highlighting the key lifestyle and environmental factors discussed that impact sperm health and fertility:
| Factor | Negative Effects on Sperm Quality | Notes |
|---|---|---|
| Air Pollution (PM2.5, SO₂, NO₂) | ↓ Motility, abnormal morphology | Linked to urban environmental exposure |
| Obesity | ↓ Sperm concentration, ↓ Motility | Hormonal and oxidative stress consequences |
| Chronic Alcohol Use | ↓ Testosterone, ↑ Estrogen, ↓ Sperm production | Hormonal disruption |
| Smoking/Tobacco | ↓ Count, ↓ Motility, ↑ DNA fragmentation | Long-term fertility risks |
| Marijuana/Recreational Drugs | ↓ Testosterone, ↓ Sperm production | Potential for long-term impacts |
| Nutrient Deficiency (Zn, Se, D) | ↓ Sperm quality | Maintain balanced, nutrient-rich diet |
| Chronic Stress | ↓ Testosterone, ↓ Sperm quality | Stress management crucial |
Healthy Sperm After a Vasectomy: What to Know
Understanding sperm health after a vasectomy requires careful consideration and ongoing monitoring. The procedure fundamentally changes reproductive dynamics, making it crucial for men to comprehend the nuanced implications. Learn more about post-vasectomy sperm management.
Sperm Clearance and Recovery Process
Following a vasectomy, sperm clearance is a complex biological process. Research from fertility specialists demonstrates significant reductions in germ cell populations, with notable decreases in pachytene spermatocytes (18%), round spermatids (40%), and elongated spermatids (39%). These cellular changes represent the body’s adaptive response to the surgical intervention.
The American Urological Association strongly recommends continuing alternative contraceptive methods until vasectomy success is definitively confirmed through post-vasectomy semen analysis (PVSA). Motile sperm can persist for several weeks post-procedure, necessitating careful monitoring and verification.
Long-Term Sperm Health Considerations
Long-term vasectomy effects on sperm health reveal fascinating biological adaptations. Scientific studies indicate that men vasectomized for over five years experience markedly reduced sperm yields. These reductions are accompanied by increased sperm DNA fragmentation, suggesting heightened apoptosis in germ cells.
Interestingly, while sperm production dramatically decreases, the body continues complex reproductive processes. Testosterone production remains unaffected, and sexual function typically remains unchanged. Comprehensive sexual health resources provide deeper insights into these physiological nuances.
Monitoring and Verification Strategies
Professional medical guidance is paramount in navigating post-vasectomy sperm health. At-home semen analysis provides a convenient and discreet method for tracking sperm clearance. Multiple analyses over several months help confirm the procedure’s effectiveness and ensure complete sperm elimination.
Key verification strategies include:
- Conducting recommended post-vasectomy semen analyses
- Maintaining consistent follow-up with healthcare providers
- Understanding individual biological variation in sperm clearance
While vasectomy represents a highly effective contraceptive method, individual experiences vary. Comprehensive monitoring, professional medical consultation, and patient awareness remain critical in achieving optimal reproductive health outcomes. Men should approach post-vasectomy care with patience, understanding that complete sperm clearance is a gradual biological process requiring careful verification.
Improving Sperm Health for Conception Success
Achieving successful conception requires a holistic approach to male reproductive health. Men can significantly enhance their fertility potential through targeted lifestyle modifications and proactive health strategies. Discover comprehensive insights into optimizing sperm function.
Physical Activity and Reproductive Wellness
Research from exercise physiologists demonstrates that regular physical activity plays a crucial role in improving sperm quality. Moderate-intensity exercises like walking and jogging can reduce DNA damage, enhance sperm morphology, and lower metabolic stress factors. The key lies in maintaining a consistent and balanced approach to physical fitness.
Interestingly, weight management studies reveal that targeted weight loss through dietary changes and increased physical activity can dramatically improve sperm parameters. By lowering systemic inflammation, reducing oxidative stress, and restoring reproductive hormone balance, men can significantly enhance their fertility potential.
Holistic Stress Reduction Techniques
Yoga research provides compelling evidence of the profound impact stress reduction can have on reproductive health. Practices like Yoga and Yoga Nidra have been associated with notable improvements in sperm count, motility, and morphology. These techniques likely work by reducing stress and enhancing blood circulation to reproductive organs.
Mental health plays an equally critical role. Chronic stress triggers hormonal cascades that can negatively impact sperm production. Implementing stress management techniques such as meditation, deep breathing exercises, and regular psychological counseling can help mitigate these negative effects. Advanced semen analysis techniques can help men track the effectiveness of these interventions.
Nutritional Strategies for Sperm Optimization
Nutrition emerges as a powerful tool in improving sperm health. Diets rich in antioxidants, omega-3 fatty acids, and essential minerals can significantly enhance sperm quality. Key nutrients include:
- Zinc, which supports testosterone production
- Selenium, crucial for sperm motility
- Vitamin D, important for overall reproductive function
- Antioxidants that protect sperm from oxidative damage
Supplementation should be approached carefully and ideally under professional medical guidance. While dietary interventions can be powerful, individual metabolic responses vary. Consulting with healthcare providers and potentially undergoing comprehensive fertility assessments can provide personalized insights.
Conception is a complex journey that requires patience, understanding, and a comprehensive approach to reproductive health. By integrating physical activity, stress management, and targeted nutrition, men can significantly improve their chances of successful conception. Regular monitoring, professional medical consultation, and a holistic lifestyle approach remain the most effective strategies for optimizing sperm health and fertility potential.
Frequently Asked Questions
What is considered a healthy sperm count?
A healthy sperm count is at least 16 million sperm per milliliter of semen. Counts below this threshold may affect fertility.
How important is sperm motility for fertility?
Sperm motility is crucial; at least 30% of sperm should exhibit progressive movement toward the egg for optimal fertility.
What lifestyle factors can negatively impact sperm health?
Factors like obesity, chronic stress, smoking, and alcohol use can significantly reduce sperm quality and fertility potential.
How can I improve my sperm health for conception?
Improving sperm health can be achieved through regular physical activity, a balanced diet rich in antioxidants and essential nutrients, and effective stress management techniques.
Recommended
- Sperm Vitality Testing: Essential Guide for Vasectomy and Fertility
- Sperm Function Tests Guide: Fertility, Vasectomy, and Beyond
- How to Read Semen Results: Vasectomy & Fertility in 2025
- Laboratory Sperm Testing: Vasectomy Results & Fertility in 2025
- Semen Analysis and Fertility Planning: Insights for Vasectomy and Conc
- Routine Semen Analysis Benefits for Vasectomy and Fertility 2025





