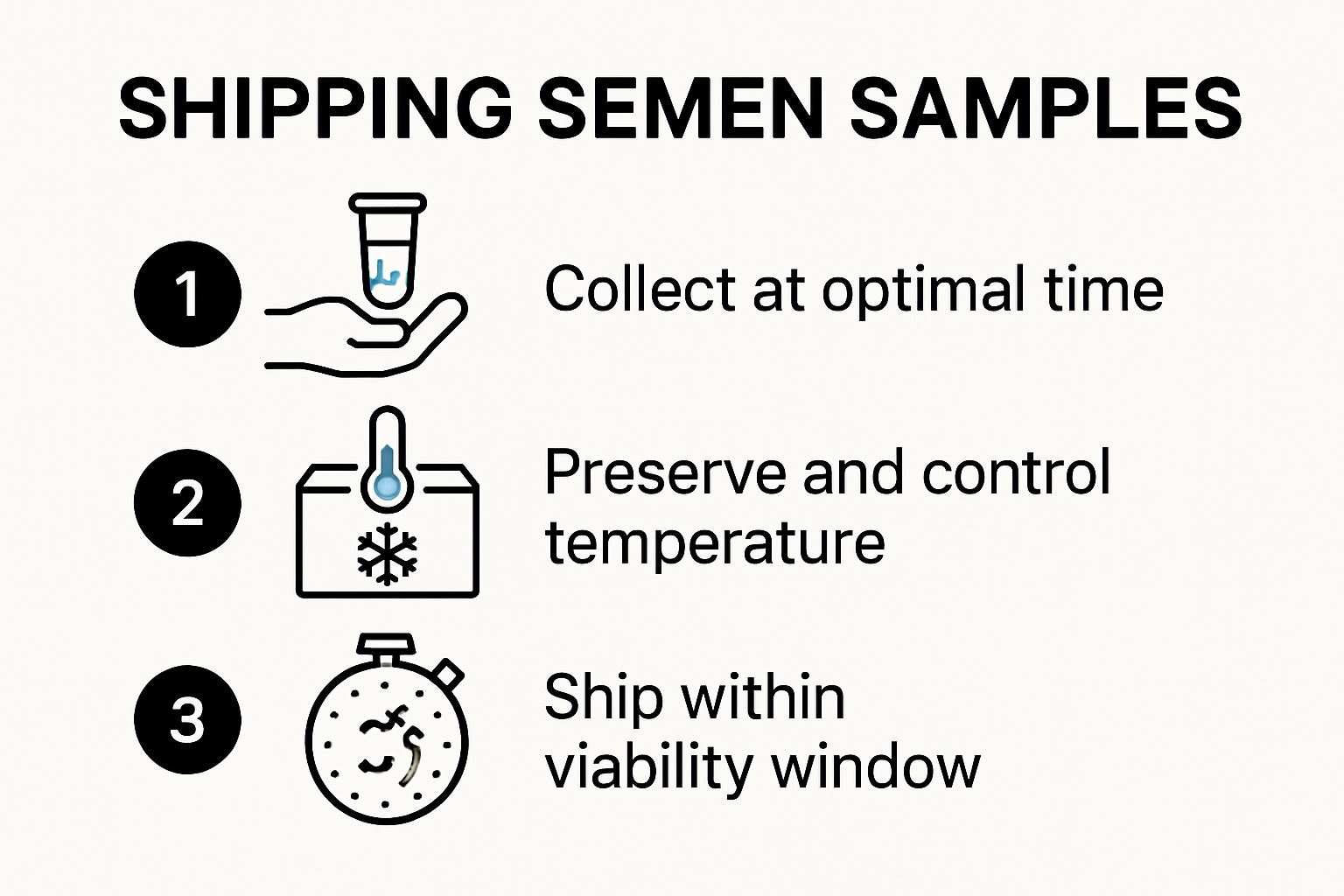
Shipping semen samples for fertility testing and medical diagnostics sounds straightforward, but the stakes are surprisingly high. Samples lose viability quickly—lab guidelines warn they should arrive within one hour of collection to ensure accuracy. Many imagine the hardest part is getting the logistics right. That’s a myth. The real challenge is the science behind preservation and meeting strict temperature controls, where just a few degrees off can ruin everything.
Table of Contents
- Understanding Why And When To Ship Semen Samples
- Preparing Semen Samples For Safe Shipping
- Choosing The Best Shipping Methods And Supplies
- Ensuring Accurate Results And Legal Compliance
Quick Summary
| Takeaway | Explanation |
|---|---|
| Timeliness is Crucial | Semen samples must be delivered to laboratories ideally within one hour of collection to maintain maximum viability and ensure accurate diagnostic results. |
| Proper Preparation is Key | Samples should be collected in sterile, medical-grade containers, ideally after 2-7 days of abstinence to maximize sperm quality and concentration. |
| Temperature Control is Essential | Maintaining samples at temperatures between 2-10 degrees Celsius during transit is critical for preserving sperm motility and overall quality. |
| Regulatory Compliance is Mandatory | Shipping semen samples requires compliance with strict packaging, labeling, and documentation standards set forth by DOT and IATA to guarantee specimen safety and quality. |
| Legal and Ethical Protections Exist | Legal frameworks, including CLIA, ensure laboratories adhere to rigorous quality standards, protecting both patient health and maintaining integrity in medical testing practices. |
Understanding Why and When to Ship Semen Samples
Shipping semen samples represents a critical process for medical diagnostics, fertility assessment, and post-vasectomy confirmation. Understanding the precise conditions and timing for sample shipment ensures accurate results and maintains the biological integrity of the specimen.
The Science Behind Semen Sample Preservation
Semen samples are delicate biological materials that require careful handling and transportation. Research from the National Institutes of Health reveals that sperm motility and viability begin to decline rapidly after collection. This means the window for shipping is narrow and critically time-sensitive. Proper preservation techniques become paramount in maintaining sample quality.
Optimal sample collection involves specific preparation. Experts recommend collecting samples after 2-7 days of sexual abstinence to ensure optimal sperm concentration and quality. The collection method matters significantly - using sterile, non-toxic containers and avoiding contamination are crucial steps in preparing a sample for shipping.
Shipping Protocols and Safety Considerations
Shipping semen samples requires meticulous attention to biological safety and transportation regulations. According to Michigan State University’s veterinary guidelines, proper packaging is essential. This involves using a leak-proof primary container, a secondary container with absorbent material, and a sturdy outer container that prevents potential biohazard exposure.
Temperature control plays a critical role in sample preservation. Most clinical protocols require maintaining the sample between 20-37 degrees Celsius during transportation. Extreme temperatures can significantly compromise sperm motility and overall sample quality. Our guide on understanding semen testing provides more insights into the scientific nuances of sample handling.
For men undergoing post-vasectomy confirmation or fertility assessments, understanding these shipping protocols eliminates potential errors. The goal is simple: deliver a viable sample that provides accurate diagnostic information. This means timing the collection, following strict handling guidelines, and ensuring rapid transportation to the laboratory.
Laboratories typically require samples to be delivered within one hour of collection to maintain maximum sperm viability. When shipping is necessary, specialized containers and rapid transportation methods become critical. Some clinics use specialized medical courier services designed specifically for biological specimen transport, ensuring the sample reaches its destination quickly and safely.
While shipping might seem straightforward, it involves complex biological and logistical considerations. Each step - from collection to transportation - can impact the ultimate diagnostic accuracy. Medical professionals and patients must work together to follow precise protocols, ensuring the most reliable results possible.
The landscape of semen sample shipping continues to evolve, with emerging technologies and improved preservation techniques making the process more reliable and accessible. For individuals navigating fertility assessments or post-surgical confirmations, understanding these intricate details can make a significant difference in their medical journey.
Here is a table summarizing key shipping protocols and safety considerations mentioned above for quick reference.
| Protocol / Consideration | Key Requirement |
|---|---|
| Leak-proof Primary Container | Prevents spills and contamination |
| Secondary Container with Absorbent Material | Contains leaks in case of breakage |
| Sturdy Outer Container | Shields sample from physical damage |
| Temperature Control | Maintain between 20-37°C (shipping); 2-10°C (preservation) |
| Rapid Transportation | Delivery typically within 1 hour of collection |
| Specialized Courier Services | Used for faster and safer delivery |
| Accurate Documentation | Includes patient ID, time of collection |
Preparing Semen Samples for Safe Shipping
Preparing semen samples for shipping requires precision, careful handling, and adherence to strict medical protocols. The process involves multiple critical steps that protect sample integrity and ensure accurate diagnostic results.
Collection and Initial Processing
Research from the World Health Organization emphasizes the importance of maintaining optimal conditions during sample preparation. Initial collection demands a sterile environment and specific techniques to minimize contamination and preserve sperm quality.
Collection containers must be medical-grade, non-toxic, and specifically designed for semen specimen transport. Clinical guidelines recommend using containers with specialized preservative media that stabilize sperm cells during transportation. These containers typically include chemical stabilizers that prevent rapid sperm degradation and maintain cellular structure.
Temperature and Preservation Strategies
Temperature management represents a crucial aspect of semen sample preparation. A comprehensive study in Fertility and Sterility demonstrated that maintaining samples between 2-10 degrees Celsius during shipping can preserve sperm motility and concentration. This requires specialized packaging that provides consistent thermal protection.
Medical professionals recommend using insulated shipping containers with temperature-control gel packs. These containers create a stable environment that minimizes temperature fluctuations during transit. Our comprehensive guide to semen test kit instructions provides detailed insights into proper packaging techniques.
Additionally, laboratories often require samples to be accompanied by specific documentation. This includes patient identification information, collection timestamp, and any relevant medical history that might impact sample analysis. Proper labeling prevents potential mix-ups and ensures accurate tracking throughout the shipping process.
Biohazard safety is another critical consideration. Semen samples must be packaged in leak-proof, sealed containers that comply with international shipping regulations for biological materials. This typically involves multiple layers of packaging - a primary container holding the sample, a secondary containment with absorbent material, and an outer shipping container marked with appropriate biohazard symbols.
Advanced Preservation Techniques
Clinical research in Theriogenology highlights emerging preservation techniques that extend sample viability. Some advanced methods involve specialized dilution media and controlled cooling protocols that minimize cellular damage during transportation.
For individuals shipping samples for fertility assessments or post-vasectomy confirmation, understanding these technical nuances can significantly impact diagnostic accuracy. The goal is not just transportation, but maintaining the biological integrity of the specimen from collection through laboratory analysis.
Technology continues to evolve, with innovations in packaging, preservation media, and transportation methods consistently improving the reliability of semen sample shipping. Medical professionals and patients alike benefit from these advancements, which make remote testing and analysis increasingly precise and accessible.
Ultimately, successful semen sample shipping requires a combination of medical expertise, careful preparation, and adherence to stringent scientific protocols. Each step - from initial collection to final delivery - plays a crucial role in ensuring the most accurate and reliable diagnostic results possible.
Below is a table outlining the main steps involved in preparing a semen sample for shipping as described in this section.
| Step | Description |
|---|---|
| Collection | Use sterile, medical-grade, non-toxic containers in a contamination-free environment |
| Initial Processing | Add specialized preservative or dilution media, stabilize sperm cells |
| Temperature Management | Maintain sample at 2–10°C using insulated containers and gel packs |
| Documentation | Prepare patient ID, collection time, and medical history paperwork |
| Biohazard Packaging | Place in leak-proof, sealed containers with absorbent material, label with biohazard symbols |
| Final Packaging | Use outer shipping container for protection and compliance |
Choosing the Best Shipping Methods and Supplies
Selecting appropriate shipping methods and supplies for semen samples is a critical process that directly impacts sample integrity, diagnostic accuracy, and overall testing reliability. The right combination of packaging, transportation, and documentation ensures the specimen remains viable from collection through laboratory analysis.
Regulatory Compliance and Packaging Standards
Research from the National Institutes of Health highlights the mandatory compliance with Department of Transportation (DOT) and International Air Transport Association (IATA) regulations for biological specimen shipping. These guidelines mandate specific packaging, labeling, and documentation requirements to guarantee safety and specimen preservation.
Shipping supplies must meet stringent medical standards. This includes using triple-layer packaging systems: a primary leak-proof container, a secondary containment with absorbent material, and a robust outer shipping container. Clinical guidelines recommend using containers specifically designed to maintain sample stability and prevent potential contamination.
Temperature Control and Transportation Techniques
Temperature management is crucial in semen sample shipping. Advanced research in specimen preservation demonstrates that maintaining samples between 2°C and 10°C requires specialized cooling technologies. This involves using phase change materials, frozen gel packs, and foil-lined polystyrene coolers equipped with temperature monitoring devices.
Different shipping methods offer unique advantages. Overnight courier services with temperature-controlled transport provide the most reliable option for maintaining sample integrity. Our comprehensive guide to semen analysis timing offers insights into selecting the most appropriate shipping method for specific diagnostic needs.
Specialized Shipping Considerations
Beyond basic packaging, specialized shipping supplies include biohazard labels, detailed tracking documentation, and temperature-sensitive indicators. Medical professionals must ensure all documentation accurately identifies the specimen, includes collection timestamps, and follows laboratory-specific submission protocols.
Shipping options range from local medical courier services to specialized biological specimen transportation networks. Each method requires careful evaluation based on factors like distance, expected transit time, and specific laboratory requirements. Some advanced shipping kits now include integrated temperature logging technologies that provide real-time tracking and preservation data.
Emerging technologies continue to revolutionize biological specimen shipping. Innovations in packaging materials, temperature-control mechanisms, and tracking systems are making remote sample transportation increasingly reliable and precise. For patients undergoing fertility assessments or post-vasectomy confirmation, these advancements mean more accessible and accurate diagnostic processes.
Choosing the right shipping method is not just about transportation - it is about preserving the scientific integrity of the specimen. Medical professionals and patients must work together to select shipping supplies and methods that meet the highest standards of safety, reliability, and diagnostic accuracy.
Ultimately, successful semen sample shipping combines medical expertise, technological innovation, and strict adherence to regulatory guidelines. Each carefully selected supply and shipping method contributes to ensuring the most accurate and dependable test results possible.
Ensuring Accurate Results and Legal Compliance
Accurate semen sample analysis and legal compliance represent critical components of modern reproductive health diagnostics. Medical professionals and patients must navigate a complex landscape of regulatory requirements, scientific standards, and ethical considerations to ensure reliable and legally sound testing processes.
Laboratory Certification and Quality Standards
The Clinical Laboratory Improvement Amendments (CLIA) establish comprehensive federal standards for clinical laboratory testing in the United States. These regulations mandate strict quality control measures, personnel qualifications, and testing protocols to guarantee the accuracy and reliability of diagnostic results.
Laboratories must undergo rigorous certification processes that involve periodic inspections, proficiency testing, and continuous quality improvement protocols. Research from medical compliance standards indicates that these certifications ensure laboratories maintain high-precision equipment, employ qualified technicians, and follow standardized analysis procedures.
Legal and Ethical Considerations in Specimen Handling
State-specific regulations provide additional layers of legal protection for patients. For instance, reproductive tissue banks must perform comprehensive screening tests, including HIV, hepatitis B and C, syphilis, and other critical infectious disease markers. These requirements protect both patient health and maintain the integrity of medical testing processes.
Privacy regulations play a crucial role in specimen management. Medical facilities must implement strict confidentiality protocols that protect patient information throughout the testing process. This includes secure documentation, limited access to sensitive medical records, and transparent consent procedures.
Comprehensive Testing and Result Verification
Accurate semen sample analysis requires multiple verification steps. Laboratories typically perform duplicate testing and cross-referencing to minimize potential errors. Our guide to understanding semen testing processes provides deeper insights into the comprehensive verification methods used in modern diagnostic protocols.
Technological advancements continue to enhance testing accuracy. Advanced microscopy techniques, automated analysis systems, and machine learning algorithms help reduce human error and provide more precise diagnostic information. These innovations contribute to more reliable results and improved patient outcomes.
Ethical considerations extend beyond technical accuracy. Medical professionals must ensure patients fully understand the testing process, potential implications of results, and their rights throughout the diagnostic journey. Informed consent, clear communication, and patient education are fundamental to maintaining trust and legal compliance.
The intersection of medical science, legal requirements, and ethical standards creates a complex but essential framework for semen sample testing. Each regulatory requirement, from laboratory certification to patient privacy protections, serves a critical purpose in safeguarding patient health and ensuring diagnostic reliability.
As reproductive health technologies continue to evolve, so too will the legal and scientific standards governing semen sample analysis. Medical professionals, policymakers, and technology developers must collaborate to create frameworks that balance scientific innovation, patient privacy, and comprehensive healthcare standards.
Frequently Asked Questions
What is the ideal time frame for shipping semen samples?
Semen samples should ideally be delivered to laboratories within one hour of collection to maintain maximum viability and ensure accurate diagnostic results.
What temperature should semen samples be maintained at during shipping?
Samples should be kept at temperatures between 2-10 degrees Celsius during transportation to preserve sperm motility and overall quality.
What are the key requirements for packing semen samples for shipment?
Semen samples must be packaged in a leak-proof primary container, a secondary container with absorbent material, and a sturdy outer container to prevent contamination and ensure safety during transport.
What regulations must be followed when shipping semen samples?
Shipping semen samples requires compliance with regulations set by the Department of Transportation (DOT) and the International Air Transport Association (IATA), including specific packaging, labeling, and documentation standards.
Recommended
- Semen Test Kit Instructions for At-Home Vasectomy Confirmation 2025
- Why Test Semen Sample: Answers for Vasectomy & Fertility 2025
- Top Challenges in Post Vasectomy Testing: 2025 Guide for Patients and
- Understanding Semen Testing Kits: A 2025 Guide for Vasectomy and Ferti
- Why Semen Testing Is Critical: Insights for Men and Clinics
- Semen Analysis Timing: Best Practices for Vasectomy and Fertility 2025





