Semen analysis is a critical component in understanding male reproductive health. It offers essential insights into fertility, yet many find the terminology baffling. But here’s the kicker. The complexity of the words used can often overshadow the real problem at hand. Without clarity, how can anyone tackle their reproductive challenges effectively? Familiarizing yourself with these terms could be the key to unlocking deeper conversations with healthcare providers and successfully navigating the path to better reproductive health.
Table of Contents
-
-
[Lifestyle And Treatment Considerations](#lifestyle-and-treatmentImage Considerations)
Quick Summary
| Takeaway | Explanation |
| Understanding Key Terms is Essential | Familiarizing yourself with semen analysis terminology, such as sperm count, motility, and morphology, is crucial for effective communication with healthcare providers about reproductive health. |
| Interpreting Results Requires Context | Although numerical values provide vital insights, they must be understood holistically, considering factors like lifestyle and underlying health conditions to accurately assess fertility potential. |
| Professional Consultation is Key | After receiving results, consult with a urologist or reproductive specialist for a comprehensive review that includes detailed explanations and recommendations for follow-up tests. |
| Lifestyle Changes Can Enhance Fertility | Adopting healthier lifestyle choices, such as improved nutrition and stress management, can positively impact sperm quality and overall reproductive health. |
| Multiple Tests Provide Better Insights | Conducting repeated semen analyses can reveal consistent patterns and rule out temporary conditions, leading to a more accurate assessment of reproductive health. |
Common words used in semen analysis
Navigating the world of semen analysis requires understanding the specialized terminology medical professionals use during fertility and reproductive health assessments. These semen analysis terms provide crucial insights into male reproductive health and potential fertility challenges.
Clinical Parameters of Semen Evaluation
Semen analysis involves measuring multiple specific parameters that offer comprehensive insights into male reproductive potential. Sperm count represents the total number of sperm cells present in one milliliter of semen, which typically ranges between 15 million to 200 million sperm per milliliter. Physicians and reproductive specialists consider this metric fundamental in assessing male fertility.
Motility emerges as another critical term in semen testing. Sperm motility describes the percentage of sperm capable of moving effectively, which directly impacts fertility potential. Healthy sperm should demonstrate progressive forward movement, enabling successful egg fertilization. Clinicians categorize motility into several grades:
-
Progressive motility: Sperm moving forward in a straight line
-
Non-progressive motility: Sperm moving but not advancing
-
Immotile sperm: Sperm showing no movement
Diagnostic Terminology in Semen Analysis
Certain specialized terms help diagnose potential reproductive challenges. Azoospermia indicates a complete absence of sperm in the ejaculate, signaling potential blockages or production issues. Oligospermia describes low sperm concentration, typically defined as fewer than 15 million sperm per milliliter. These clinical terms provide precise diagnostic language for understanding male reproductive health.
The morphology assessment represents another crucial evaluation. Sperm morphology examines the physical shape and structure of sperm cells, determining their potential fertility effectiveness. Normal morphology involves assessing sperm head, midpiece, and tail structures. According to Mayo Clinic, abnormal morphology can significantly impact reproductive capabilities.
Additional Important Semen Analysis Terminology
Beyond clinical parameters, several additional terms provide context in semen testing. Seminal volume measures the total amount of fluid produced during ejaculation, typically ranging between 1.5 to 5 milliliters. Liquefaction time describes how quickly semen transitions from a gel-like state to a liquid consistency, which normally occurs within 20-30 minutes after ejaculation.
Understanding these semen analysis terms empowers individuals to communicate effectively with healthcare providers and comprehend their reproductive health assessments. Whether preparing for fertility treatments or conducting routine reproductive health screenings, familiarity with these clinical terms provides valuable insights into male reproductive potential.
By demystifying these specialized terms, patients can engage more confidently in discussions about their reproductive health, transforming complex medical language into clear, actionable information. 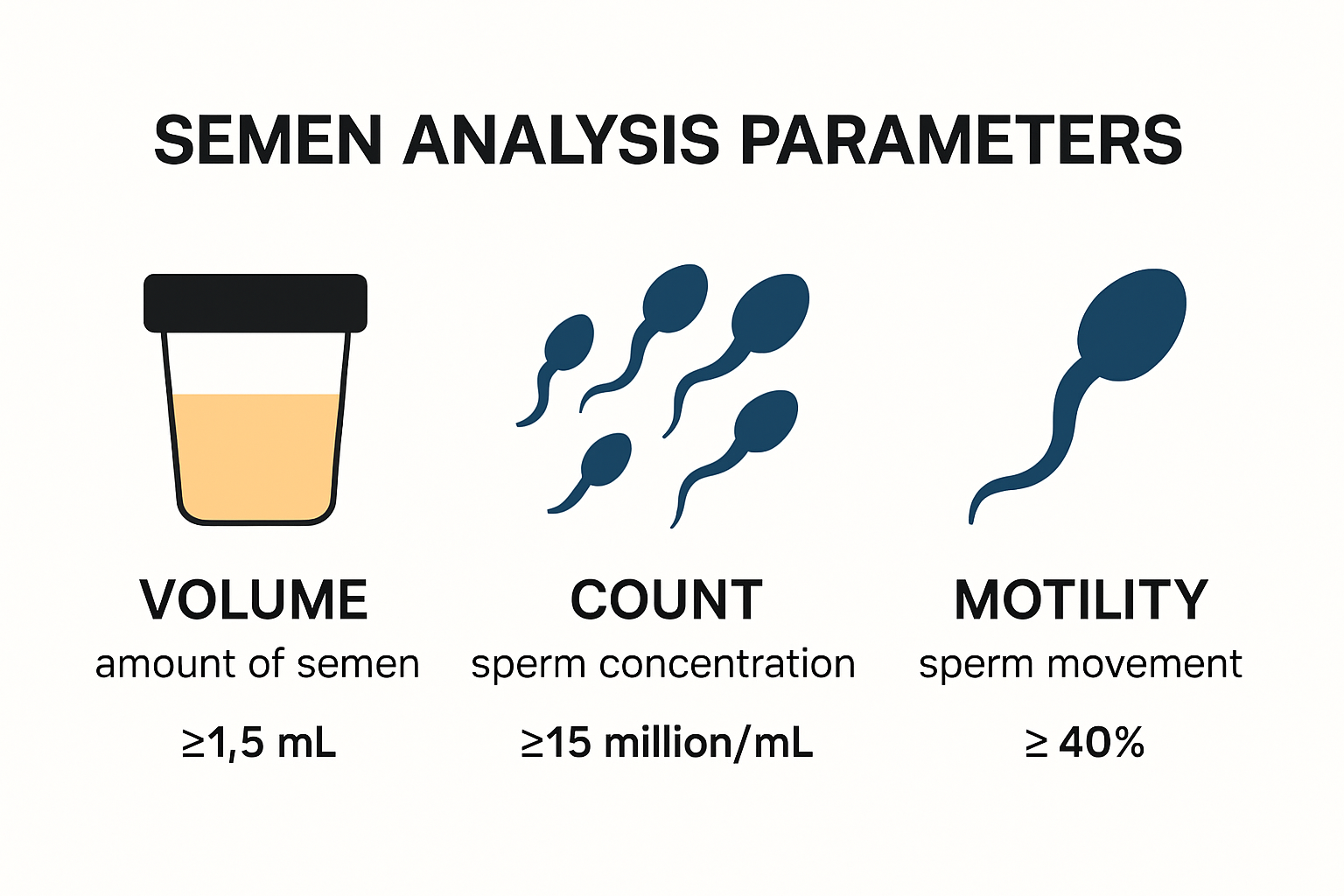
Understanding what the numbers mean
Semen analysis results can appear complex and overwhelming, with multiple numerical parameters that require careful interpretation. Understanding these numbers helps patients and healthcare providers accurately assess male reproductive health and potential fertility challenges.
Reference Ranges and Clinical Significance
Each numerical value in a semen analysis report represents a specific aspect of sperm health and reproductive potential. According to the World Health Organization, standardized reference ranges provide critical benchmarks for evaluating male fertility. Sperm concentration serves as a primary indicator, with normal ranges typically considered 15 million sperm per milliliter or higher.
Breakdown of key numerical parameters reveals nuanced insights:
-
Total sperm count: Reflects the total number of sperm in the entire ejaculate
-
Sperm motility percentage: Indicates the proportion of actively moving sperm
-
Morphology percentage: Measures the number of normally shaped sperm
Interpreting Below Normal Values
Numbers falling below established reference ranges do not automatically signify infertility but warrant further investigation. Oligospermia, characterized by low sperm concentration, might indicate potential reproductive challenges. According to Mayo Clinic, values below 15 million sperm per milliliter suggest reduced fertility potential.
Sperm motility numbers provide additional critical information. The percentage of progressively motile sperm directly impacts fertilization potential. Research from American Society for Reproductive Medicine suggests that less than 32% progressive motility can significantly reduce conception chances.
Context and Comprehensive Assessment
Numeric results must be interpreted holistically, considering multiple factors beyond isolated measurements. Morphology percentages offer insights into sperm structural quality. While normal ranges typically require at least 4% normally shaped sperm, individual reproductive capabilities vary.
Seminal volume numbers also play a crucial role. Normal ejaculate volumes range between 1.5 to 5 milliliters. Volumes consistently below 1.5 milliliters might indicate potential underlying reproductive system issues requiring further medical evaluation.
Healthcare providers emphasize that semen analysis numbers represent a snapshot of reproductive health. Multiple tests over time provide more comprehensive insights, accounting for natural variations in sperm production and quality. Factors like recent illness, stress, and lifestyle can temporarily impact semen parameters.
Patients should approach semen analysis results collaboratively with healthcare professionals. Understanding these numbers empowers individuals to make informed decisions about reproductive health, potential treatments, and fertility strategies. Professional guidance transforms complex numerical data into actionable insights, supporting comprehensive reproductive health management.
Important terms to discuss
When discussing semen analysis results with healthcare providers, understanding specific clinical terminology helps patients navigate complex reproductive health conversations more effectively. These important terms provide critical context for interpreting male fertility assessments and potential reproductive challenges.
Clinical Diagnostic Terms
Certain specialized terms help medical professionals precisely describe reproductive health conditions. Azoospermia represents a complete absence of sperm in the ejaculate, which might indicate blockages or production issues within the reproductive system. Oligospermia describes low sperm concentration, typically defined as fewer than 15 million sperm per milliliter. These diagnostic terms enable targeted medical interventions.
Additional important diagnostic categories include:
-
Asthenospermia: Reduced sperm motility affecting fertility potential
-
Teratospermia: Abnormal sperm morphology
-
Cryptozoospermia: Very low numbers of sperm requiring specialized detection techniques
Physiological Performance Indicators
Some terms directly relate to sperm performance and reproductive potential. Progressive motility specifically describes sperm moving forward in a straight line, which is crucial for successful fertilization. According to American Urological Association, progressive motility represents a key indicator of sperm quality and fertility potential.
Sperm vitality measures the percentage of live sperm in an ejaculate, which becomes particularly important when assessing samples with low motility. Research from Mayo Clinic indicates that even non-motile sperm might retain fertilization potential if they remain alive.
Laboratory and Technical Terminology
Advanced semen analysis involves specialized technical terms that describe examination methodologies. Computer-Aided Sperm Analysis (CASA) represents a sophisticated technological approach to evaluating sperm characteristics. This automated system provides precise measurements of sperm concentration, motility, and morphology.
Sperm DNA fragmentation emerges as another critical assessment, measuring potential genetic damage within sperm cells. According to National Institutes of Health, high DNA fragmentation can significantly impact fertility and embryo development, even when standard semen parameters appear normal.
Understanding these terms transforms complex medical language into actionable insights. Patients who familiarize themselves with this terminology can engage more confidently with healthcare providers, ask informed questions, and participate actively in their reproductive health management.
While these terms might initially seem intimidating, they represent powerful tools for understanding male reproductive health. Each term provides a specific lens through which medical professionals can assess fertility potential, diagnose challenges, and develop targeted treatment strategies. Open communication and mutual understanding between patients and healthcare providers remain paramount in navigating reproductive health successfully.
Next steps after your results
Receiving semen analysis results can feel overwhelming, but understanding the appropriate next steps helps transform medical data into actionable reproductive health strategies. Professional guidance becomes crucial in interpreting results and developing personalized approaches to addressing potential fertility challenges.
Professional Consultation and Interpretation
After obtaining semen analysis results, scheduling a comprehensive consultation with a urologist or reproductive specialist represents the most critical initial step. Comprehensive review involves more than simply reading numbers. According to American Urological Association, healthcare providers will evaluate results holistically, considering multiple factors beyond isolated measurements.
Key aspects of professional consultation include:
-
Detailed explanation of each numerical parameter
-
Contextual interpretation of results
-
Assessment of potential underlying health conditions
-
Recommendation of potential follow-up tests
Potential Diagnostic Follow-Up
Depending on initial results, healthcare providers might recommend additional diagnostic procedures. Repeat testing often provides more comprehensive insights, as single semen analysis results can fluctuate due to various factors. Mayo Clinic recommends multiple tests to establish consistent patterns and rule out temporary conditions.
Potential follow-up diagnostics might include:
-
Hormonal blood tests
-
Genetic screening
-
Testicular ultrasound
-
Specialized sperm function tests
Lifestyle and Treatment Considerations
Results may prompt recommendations for lifestyle modifications or potential treatment interventions. Lifestyle optimization can significantly impact reproductive health. Research from Cleveland Clinic suggests that dietary changes, stress reduction, and environmental factor management can improve sperm quality.
Potential recommendations might include:
-
Nutritional counseling
-
Exercise modifications
-
Stress management techniques
-
Potential medical interventions
Patients should approach these recommendations collaboratively with healthcare providers. Understanding that semen analysis results represent a snapshot of reproductive health empowers individuals to make informed decisions. Each result provides an opportunity for proactive health management rather than a definitive limitation.
While abnormal results might initially cause anxiety, modern reproductive medicine offers numerous strategies for addressing potential challenges. Open communication, professional guidance, and a comprehensive approach transform medical data into pathways for reproductive health optimization. Remember that a single test does not define fertility potential but instead offers valuable insights for personalized medical strategy.
Frequently Asked Questions
What is a semen analysis and why is it important?
Semen analysis is a laboratory test that evaluates various parameters of a man’s semen and sperm, providing insights into male fertility and reproductive health. It helps identify potential fertility issues.
What do the terms ‘azoospermia’ and ‘oligospermia’ mean in semen analysis?
Azoospermia refers to the complete absence of sperm in the ejaculate, while oligospermia indicates a low sperm count, typically defined as fewer than 15 million sperm per milliliter, both of which can affect fertility.
How should I interpret semen analysis results?
Interpreting semen analysis results requires understanding various parameters such as sperm concentration, motility, and morphology. Consulting with a healthcare provider is crucial for accurate context and comprehensive assessment.
What lifestyle changes can improve sperm quality?
Improving sperm quality can be achieved through lifestyle changes such as maintaining a healthy diet, managing stress, avoiding tobacco and excessive alcohol, and engaging in regular physical activity.






