Vasectomy is often viewed as a straightforward solution for permanent birth control. It involves interrupting the sperm transportation process, promising a reliable long-term contraception choice with a failure rate below 1%. But here’s the kicker: many men don’t realize that achieving true sterility doesn’t happen immediately after the procedure. In fact, post-vasectomy semen analysis is essential to confirm success and ensure zero sperm presence before abandoning alternative contraception methods. Understanding this process can make all the difference in peace of mind and confidence in your reproductive choices.
Table of Contents
Quick Summary
| Takeaway | Explanation |
| Vasectomy is a permanent contraception method | The procedure interrupts sperm transportation, providing a reliable long-term solution with minimal complications and high success rates, though it does not result in immediate sterility. |
| Post-vasectomy semen analysis is crucial | Multiple semen tests over 2-3 months are necessary to confirm azoospermia, ensuring zero or near-zero sperm presence before discontinuing alternative contraception. |
| Understanding test results is essential | Azoospermia is the ideal outcome; however, continued contraception is recommended until confirmed by a urologist, as a small pregnancy risk remains. |
| Myths about vasectomy should be addressed | Common misconceptions include impacts on sexual function and health risks; however, vasectomy does not affect testosterone levels, sexual desire, or risk of long-term health issues. |
| Regular health check-ups are advised | Post-vasectomy men should have periodic health evaluations to monitor reproductive health, despite the procedure being highly effective as a contraceptive method. |
Understand the Vasectomy Procedure
A vasectomy represents a permanent male contraception method that interrupts sperm transportation, effectively preventing pregnancy. This surgical procedure offers men a reliable long-term birth control solution with minimal complications and high success rates.
How the Vasectomy Works
The vasectomy procedure targets the vas deferens, two small tubes that transport sperm from the testicles to the urethra. During the surgical intervention, a urologist makes small incisions or punctures in the scrotum to access these tubes. The surgeon then cuts, seals, or blocks the vas deferens, preventing sperm from mixing with semen during ejaculation.
According to American Urological Association, the procedure typically takes 15-30 minutes and can be performed under local anesthesia. Most men experience minimal discomfort and can return to normal activities within a few days.
Recovery And Initial Contraception Requirements
Contrary to popular misconception, a vasectomy does not produce immediate sterility. National Institutes of Health emphasizes that residual sperm can remain in the reproductive tract for several weeks or months after the procedure. Patients must continue using alternative contraception methods and undergo post-vasectomy semen analysis (PVSA) to confirm complete sterility.
The confirmation process typically involves:
-
Multiple semen tests over 2-3 months
-
Analyzing sperm count and motility
-
Ensuring zero or near-zero sperm presence in ejaculate
While vasectomies are extremely effective, with a failure rate below 1%, rare instances of spontaneous reconnection can occur. Regular post-procedure testing ensures maximum contraceptive reliability. Healthcare providers recommend patients maintain open communication and follow recommended testing protocols to guarantee successful sterilization.
Patients should anticipate a comprehensive consultation with their urologist, who will discuss individual medical history, potential risks, and detailed post-surgical expectations. Understanding the procedure’s nuances helps men make informed decisions about this permanent contraception method.
Semen Analysis: The Gold Standard
Post-vasectomy semen analysis represents the most critical step in confirming male sterilization, serving as the definitive method to verify the success of a vasectomy procedure. This comprehensive testing process provides men and their partners with concrete evidence of reproductive effectiveness.
Understanding Post-Vasectomy Semen Analysis
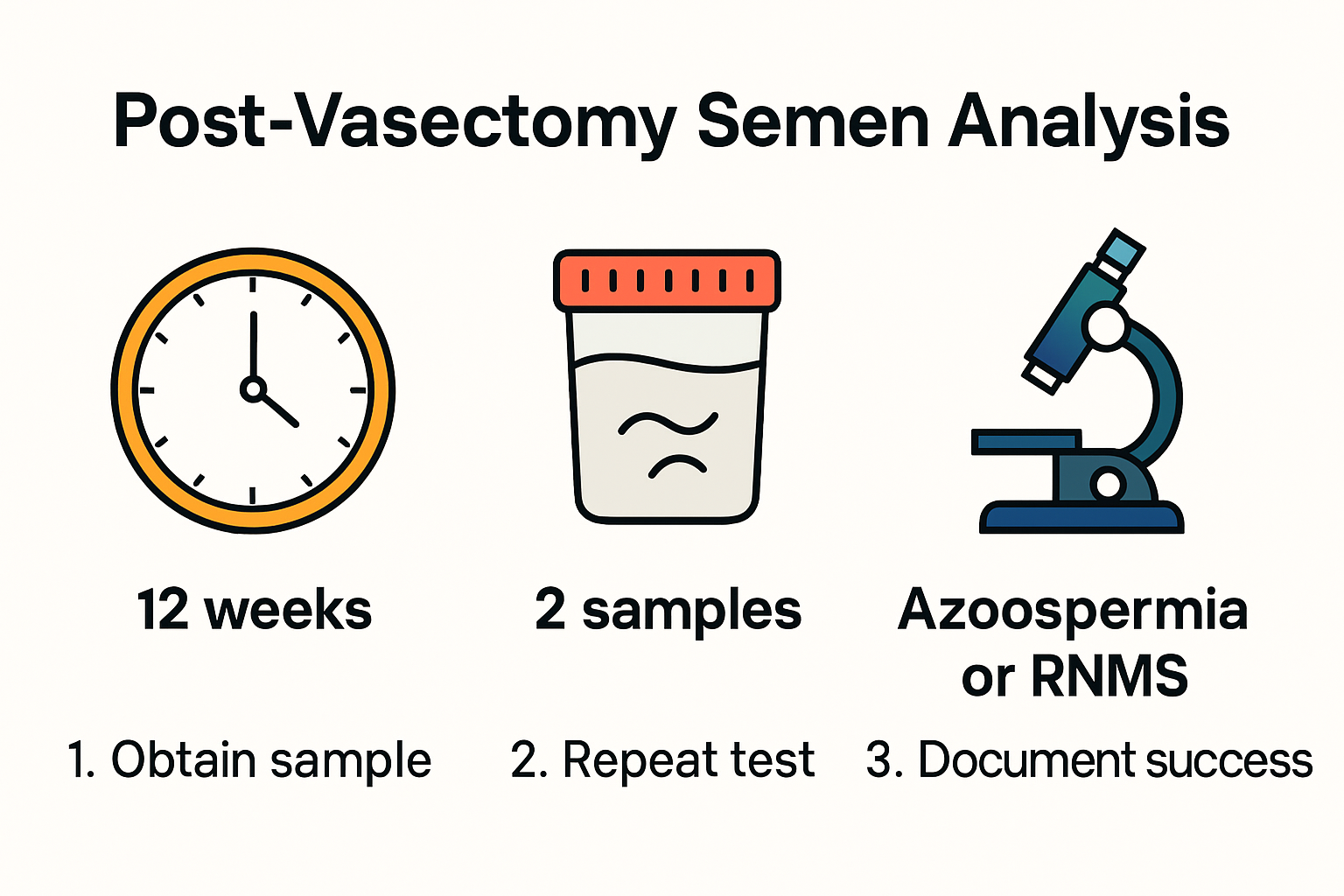
Semen analysis after a vasectomy is not a single test but a strategic process designed to thoroughly evaluate sperm presence and concentration. American Urological Association recommends multiple sample evaluations to ensure accurate results. The primary goal is to confirm azoospermia - the complete absence of sperm in the ejaculate.
Typically, healthcare providers require patients to submit 1-2 semen samples, with the first analysis conducted approximately 8-16 weeks after the vasectomy. This timing allows sufficient healing and ensures residual sperm have been cleared from the reproductive tract. According to Cambridge University Hospitals, the standard success criteria include either total sperm absence or fewer than 100,000 non-motile sperm per milliliter.
Interpreting Semen Analysis Results
 The semen analysis process involves microscopic examination of a fresh, uncentrifuged sample to detect sperm presence and characteristics. Research published in Diagnostics indicates that approximately 95.7% of first post-vasectomy analyses meet the success criteria. However, men should understand that a single negative result does not guarantee complete sterility.
The semen analysis process involves microscopic examination of a fresh, uncentrifuged sample to detect sperm presence and characteristics. Research published in Diagnostics indicates that approximately 95.7% of first post-vasectomy analyses meet the success criteria. However, men should understand that a single negative result does not guarantee complete sterility.
Critical considerations in semen analysis include:
-
Sperm count evaluation
-
Sperm motility assessment
-
Identification of any remaining sperm
University of North Carolina Urology highlights an important statistic: even after confirmed negative tests, there remains a 1 in 2000 chance of potential pregnancy. This underscores the importance of multiple follow-up analyses and continued vigilance.
Patients must follow specific guidelines for semen collection, including abstaining from ejaculation for 2-5 days before the test and carefully following laboratory submission instructions. The analysis requires precision and careful handling to ensure accurate results that provide peace of mind regarding contraceptive effectiveness.
What to Expect After Testing
After completing post-vasectomy semen analysis, men enter a critical phase of confirming their contraceptive status. Understanding the potential outcomes and next steps is essential for making informed decisions about reproductive health and contraception.
Interpreting Test Results
Post-vasectomy semen analysis results typically fall into three primary categories. American Urological Association provides clear guidelines for interpreting these outcomes. Azoospermia represents the ideal scenario, indicating zero sperm presence in the semen sample. Rare Non-Motile Sperm (RNMS) suggests minimal sperm activity, which might still be considered acceptable. However, samples showing significant sperm concentration require additional testing or potential re-intervention.
AUA Journal Research reveals an important insight: most men with fewer than 100,000 nonmotile sperm per milliliter do not develop motile sperm in subsequent analyses. This finding provides reassurance for men with borderline test results.
Continued Contraception and Follow-Up
Despite successful testing, men must maintain vigilance. University of North Carolina Urology emphasizes that a small pregnancy risk of 1 in 2,000 remains even after confirmed negative tests. Patients should continue using alternative contraception methods until their healthcare provider definitively confirms sterility.
Recommended follow-up strategies include:
-
Scheduling multiple semen analyses
-
Consulting with a urologist about individual test results
-
Maintaining open communication with sexual partners
Long-Term Considerations
Successful vasectomy confirmation does not eliminate the need for periodic reproductive health check-ups. While the procedure provides highly effective contraception, men should still undergo regular medical examinations. Potential long-term considerations include monitoring for any unusual symptoms, understanding potential hormonal changes, and maintaining overall reproductive health.
Patients should approach post-vasectomy testing as a comprehensive process, recognizing that thorough follow-up and professional medical guidance are crucial for ensuring optimal outcomes. Communication with healthcare providers and a proactive approach to understanding test results can provide peace of mind and confidence in the vasectomy’s effectiveness.
Addressing Your Concerns
Navigating the post-vasectomy period can generate numerous questions and concerns for men. Understanding common anxieties and misconceptions helps patients approach their reproductive health with confidence and clarity.
Psychological and Physical Concerns
Many men experience apprehension about potential changes in sexual function and overall masculinity after a vasectomy. American Urological Association emphasizes that a vasectomy does not affect testosterone production, sexual desire, or erectile function. The procedure exclusively interrupts sperm transportation, leaving hormonal and sexual responses entirely unchanged.
Journal of Sexual Medicine research indicates that most men report no significant difference in sexual satisfaction after vasectomy. In fact, many couples experience improved intimacy due to reduced pregnancy anxiety and eliminated contraceptive concerns.
Medical Misconceptions and Realities
Clinical evidence addresses several persistent myths surrounding vasectomy. AUA Journal Research provides critical insights into patient concerns, particularly regarding nonmotile sperm detection during post-procedure testing. Surprisingly, the presence of nonmotile sperm does not indicate procedure failure and should not trigger unnecessary anxiety.
Common misconceptions include:
-
Vasectomy reduces sexual performance
-
The procedure causes immediate sterility
-
Nonmotile sperm means the vasectomy was unsuccessful
-
Testosterone levels will decrease
Long-Term Health Considerations
Contrary to popular belief, vasectomy does not increase health risks. National Institutes of Health studies demonstrate no significant correlation between vasectomy and prostate cancer, cardiovascular diseases, or other long-term health complications. The procedure remains a safe, reliable contraceptive method with minimal medical risks.
Patients should maintain open communication with healthcare providers, ask detailed questions, and approach the procedure with accurate information. Understanding the medical science behind vasectomy helps reduce anxiety and supports informed decision-making about reproductive health. Every individual’s experience is unique, and personalized medical guidance remains the most reliable source of accurate information.
Frequently Asked Questions
How long after a vasectomy can I confirm its success?
You can confirm the success of a vasectomy typically 8-16 weeks after the procedure through a post-vasectomy semen analysis (PVSA), which tests for the absence of sperm in your semen.
What is a post-vasectomy semen analysis?
A post-vasectomy semen analysis is a test conducted after vasectomy to determine if sperm is present in the semen, confirming whether the procedure was successful in achieving azoospermia, the complete absence of sperm.
How many tests do I need after a vasectomy?
Patients generally need to submit 1-2 semen samples, usually over a period of 2-3 months, to ensure accurate results and confirm complete sterility.
Can a vasectomy fail after initial testing shows success?
Yes, even after initial testing shows no sperm present, there is a small chance of failure. Statistics indicate about a 1 in 2,000 risk of pregnancy, which is why continued use of alternative contraception is recommended until definitive confirmation from a healthcare provider.





