Thinking a vasectomy means instant sterility is a common mistake. Here is the catch. Up to 30 percent of men skip the required follow-up semen test after surgery, risking unexpected pregnancies. What surprises many is that sperm can stick around for weeks or even months after the procedure. Knowing this can turn a simple test into your most important step for true peace of mind.
Table of Contents
- Understanding Semen Testing After Vasectomy
- Preparing For Your Semen Sample Collection
- Interpreting Semen Analysis Results Together
- Common Questions About Semen Testing And Fertility
Quick Summary
| Takeaway | Explanation |
|---|---|
| Post-Vasectomy Semen Testing is Essential | Confirming successful vasectomy effectiveness is crucial and should be done through semen analysis 8 to 16 weeks post-procedure to ensure the absence of sperm (azoospermia). |
| Strict Guidelines for Sample Collection | Proper sample collection techniques including timing (48 to 7 days abstinence) and methods (collecting entire ejaculate) are vital for obtaining accurate testing results. |
| Continuous Use of Contraception Until Confirmation | Men must use alternative contraception methods until receiving a confirmed negative sperm analysis report, as sperm can linger in the reproductive tract for weeks or months after vasectomy. |
| Understanding Results is a Collaborative Process | Interpreting semen analysis results requires discussions with healthcare providers, focusing on sperm count, motility, and follow-up recommendations for ongoing reproductive health. |
| Address Psychological Aspects | Men’s emotional well-being is important; addressing anxieties and maintaining open communication with partners can help alleviate concerns related to the testing process. |
Understanding Semen Testing After Vasectomy
Vasectomy is a highly effective form of permanent male contraception, but confirming its success requires precise follow-up through semen testing. Patient education semen testing plays a crucial role in verifying the procedure’s effectiveness and ensuring men can confidently stop using alternative contraception methods.
The Science Behind Post Vasectomy Verification
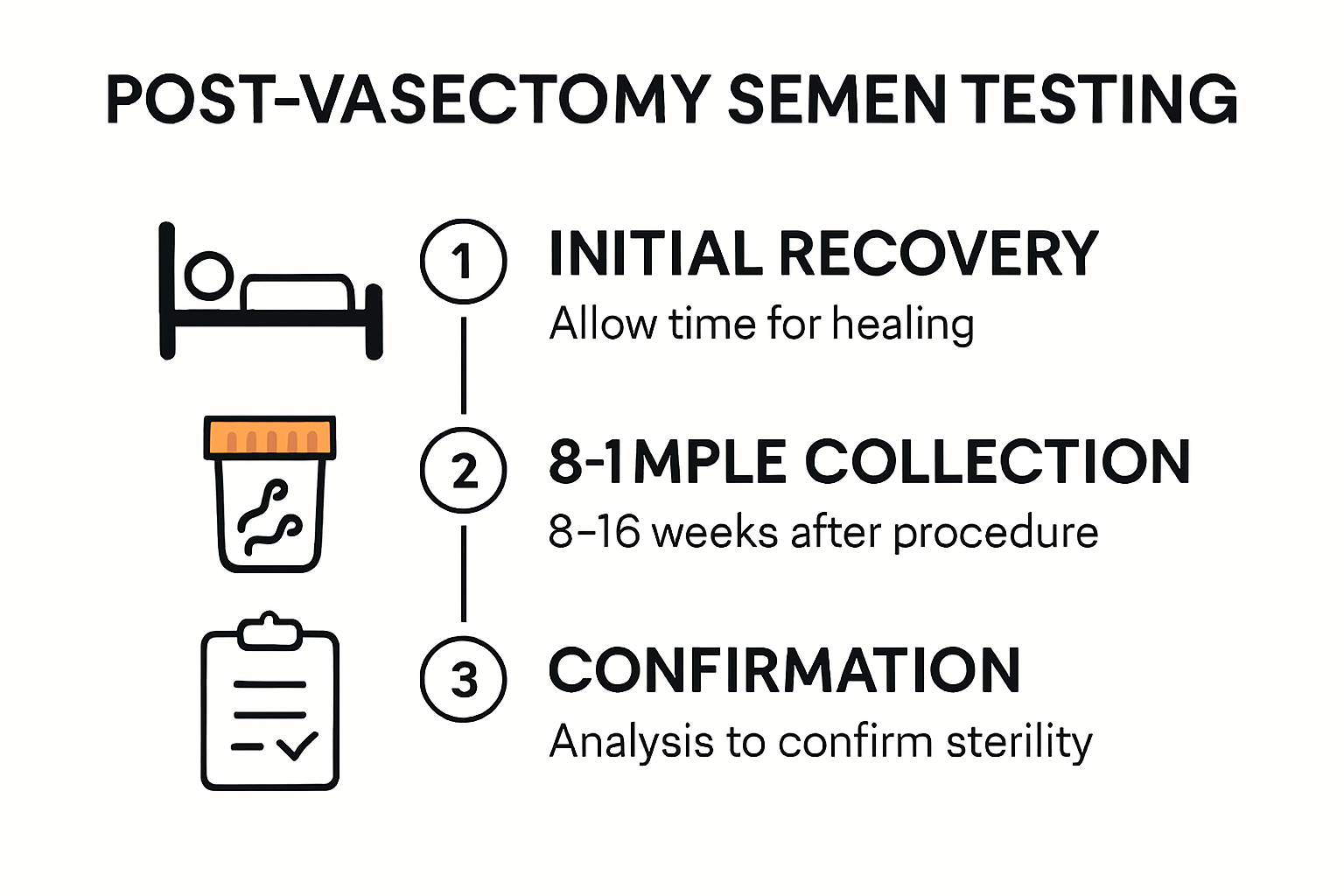
After a vasectomy, the body does not immediately become sterile. The surgical procedure blocks sperm from traveling through the vas deferens, but residual sperm can remain in the reproductive tract. Research from the CDC recommends performing a semen analysis 8 to 16 weeks post-procedure to confirm complete azoospermia (absence of sperm).
The testing process involves a comprehensive examination of the ejaculate. Urological experts recommend analyzing a fresh, uncentrifuged semen sample within two hours of collection to accurately assess sperm motility and concentration. This detailed analysis ensures precise confirmation of the vasectomy’s success.
Patient Compliance and Testing Protocols
Compliance with post-vasectomy semen testing remains a significant challenge in reproductive healthcare. Clinical studies have revealed that up to 30% of men fail to submit a single follow-up sample, potentially compromising their contraceptive reliability. This statistic underscores the critical need for clear patient education and streamlined testing processes.
Men must understand that continuing to use alternative contraception is essential until a confirmed negative sperm count is documented. Learn more about why testing is critical for vasectomy confirmation.
The testing protocol typically involves multiple steps. Initially, patients collect a semen sample either at home or in a clinical setting. The sample undergoes microscopic examination to count and assess sperm. Multiple tests might be required to confirm complete sterility, as sperm can persist in the reproductive tract for weeks or months after the procedure.
Modern testing solutions have transformed this process, offering men discreet and convenient options for post-vasectomy verification. At-home testing kits provide a comfortable alternative to traditional clinical settings, allowing men to complete this important medical follow-up with minimal disruption to their daily lives.
Understanding the importance of semen testing after a vasectomy is not just about confirming sterility—it’s about taking proactive control of one’s reproductive health. By following recommended testing protocols and working closely with healthcare providers, men can ensure the long-term effectiveness of their chosen contraceptive method.
Preparing for Your Semen Sample Collection
Collecting a semen sample for post-vasectomy testing requires careful preparation and attention to specific guidelines. The accuracy of your patient education semen testing depends on following precise protocols that ensure the most reliable results.
Optimal Timing and Abstinence Guidelines
Preparing for semen sample collection begins with understanding the critical timing requirements. Research from NHS hospitals recommends a specific abstinence period of 48 to 7 days before sample collection. This window ensures an optimal sperm count and provides the most accurate assessment of your vasectomy’s effectiveness.
Timing is crucial. Too short an abstinence period may not provide a comprehensive view of your reproductive status, while too long a period can affect sperm motility and concentration. Men should carefully track their last ejaculation to meet the recommended guidelines.
Collection Method and Sample Handling
Clinical experts at Cambridge University Hospitals emphasize the importance of collecting the entire ejaculate through masturbation directly into a sterile, non-toxic container. The first portion of the ejaculate contains the highest concentration of sperm, making complete collection critical for accurate analysis.
Cleveland Clinic guidelines stress the importance of sample transportation. The specimen must be delivered to the laboratory within one hour of collection and maintained at body temperature. This ensures the most accurate assessment of sperm motility and overall sample quality.
Preparing for At-Home Testing
Modern at-home testing solutions have simplified the semen collection process. Learn more about our comprehensive test kit instructions to ensure you complete the process correctly.
Prepare your testing environment in advance. Ensure privacy, have all collection materials ready, and carefully read the instructions provided with your testing kit. Avoid using lubricants or condoms not specifically approved for semen analysis, as these can interfere with sample quality.
Some additional preparation tips include staying hydrated, avoiding alcohol and tobacco for 24-48 hours before collection, and maintaining a consistent sleep schedule. These factors can subtly impact sperm quality and testing accuracy.
Mental preparation is equally important. The testing process can cause anxiety for some men, so approach the collection calmly and follow the provided instructions precisely. Remember that this test is a crucial step in confirming the success of your vasectomy and providing peace of mind.
If you encounter any difficulties during sample collection or have concerns about the process, consult your healthcare provider. They can provide personalized guidance and address any specific questions or challenges you might experience during post-vasectomy semen testing.
Interpreting Semen Analysis Results Together
Patient education semen testing results require careful and precise interpretation. Understanding the nuanced details of your post-vasectomy semen analysis can help you confidently navigate the next steps in your reproductive health journey.
Understanding Sperm Count and Motility Criteria
The American Urological Association provides clear guidelines for interpreting vasectomy success. The primary benchmark for a successful vasectomy is achieving azoospermia or having ≤100,000 non-motile sperm per milliliter. This stringent criteria ensures that the risk of potential pregnancy is minimized.
Research from the Canadian Urological Association suggests that if motile sperm or more than 100,000 non-motile sperm persist beyond six months post-vasectomy, a repeat vasectomy procedure might be recommended. This highlights the importance of thorough and repeated testing.
Timing and Follow-up Recommendations
The British Andrology Society recommends a comprehensive approach to post-vasectomy testing. They advise conducting the initial semen analysis 16 weeks after the procedure, following at least 24 ejaculations. Complete clearance is granted only after two consecutive sperm-free ejaculates.
Learn more about decoding your semen analysis results to understand the nuances of your specific test outcomes.
Counseling and Contraceptive Considerations
Interpretation of semen analysis results is not just about numbers. Healthcare providers play a crucial role in counseling patients about the implications of their results. In cases of persistent non-motile sperm, patients require detailed guidance on continuing alternative contraceptive methods.
Patients should approach result interpretation as a collaborative process. Discussing results with a healthcare professional allows for personalized interpretation, addressing any concerns or questions about fertility status, potential risks, and future reproductive choices.
Key factors to consider during result interpretation include:
- Total sperm count
- Sperm motility
- Presence of non-motile sperm
- Timing since vasectomy procedure
- Individual health considerations
Remember that each semen analysis is unique. While standardized guidelines provide a framework, individual variations can occur. Open communication with your healthcare provider ensures a comprehensive understanding of your specific results.
Psychological preparation is equally important. Waiting for and interpreting semen analysis results can be anxiety-inducing. Approaching the process with patience, understanding, and professional guidance can help manage emotional aspects of post-vasectomy testing.
Ultimately, semen analysis results are a critical tool in confirming the success of your vasectomy. By understanding the scientific criteria, following recommended testing protocols, and maintaining open communication with healthcare professionals, you can confidently navigate this important phase of reproductive health management.
Common Questions About Semen Testing and Fertility
Patient education semen testing involves numerous questions and concerns that men frequently encounter during their post-vasectomy journey. Understanding these common inquiries can help alleviate anxiety and provide clarity about the testing process and fertility implications.
Timing and Frequency of Testing
Research from the National Institutes of Health recommends conducting the initial post-vasectomy semen analysis between 8 to 16 weeks after the procedure. This specific timeframe allows sufficient time for the reproductive system to clear remaining sperm and provides an accurate assessment of vasectomy effectiveness.
The American Urological Association guidelines emphasize that patients must continue using alternative contraceptive methods until vasectomy success is definitively confirmed. A single analysis demonstrating azoospermia (no sperm) or rare non-motile sperm (≤100,000 sperm/mL) is typically sufficient to establish sterility.
Understanding Potential Fertility Concerns
Men often wonder about the long-term implications of vasectomy on their reproductive health. Explore comprehensive insights about sperm function and fertility testing to gain a deeper understanding of these nuanced medical considerations.
Common questions include:
- Will the vasectomy impact my hormone levels?
- Can sperm production be restored if I change my mind?
- Are there potential long-term health effects?
Medical experts reassure patients that vasectomy primarily affects sperm transportation, not overall hormone production or sexual function. Testosterone levels remain unchanged, and sexual performance typically continues without interruption.
Addressing Psychological and Emotional Aspects
Beyond medical considerations, patients frequently express psychological concerns about semen testing and fertility. The process can trigger anxiety about masculinity, future reproductive choices, and personal identity.
Healthcare professionals recommend approaching semen testing with open communication and a supportive mindset. Partners should engage in collaborative discussions, understanding that the procedure is a mutual decision about family planning.
Key emotional considerations include:
- Managing potential feelings of loss or uncertainty
- Maintaining open communication with partner
- Seeking professional counseling if experiencing significant emotional distress
Interestingly, clinical studies indicate that most men report increased satisfaction and reduced anxiety after completing post-vasectomy semen testing, confirming the procedure’s effectiveness.
Patients should remember that patient education semen testing is a proactive health management strategy. It provides concrete information, eliminates uncertainty, and empowers individuals to make informed reproductive health decisions.
While questions and concerns are natural, approaching semen testing with knowledge, professional guidance, and a supportive network can transform the experience from potentially stressful to genuinely informative and reassuring.
Below is a table summarizing the step-by-step protocol for semen sample collection and testing after a vasectomy, based on current best practices discussed in the article:
| Step | Description | Key Details |
|---|---|---|
| 1 | Follow Abstinence Guidelines | 48 hours to 7 days since last ejaculation before sample collection |
| 2 | Collect Entire Ejaculate | Masturbate into a sterile, non-toxic container; collect entire sample |
| 3 | Proper Sample Handling | Do not use lubricants/condoms unless approved; ensure privacy and preparation |
| 4 | Transport Sample Promptly | Deliver to lab within 1 hour; keep at body temperature |
| 5 | Laboratory Analysis | Analyze sample within two hours of collection for motility and count |
| 6 | Repeat Testing If Needed | Follow provider recommendations for additional tests as required |
To help clarify when and how to interpret post-vasectomy semen testing results, the next table compares major clinical guideline recommendations referenced in the article:
| Organization | When to Test | Criteria for Success | Next Steps If Sperm Present |
|---|---|---|---|
| CDC & NIH | 8–16 weeks post-vasectomy | Azoospermia or ≤100,000 non-motile sperm/mL | Retest, possibly repeat vasectomy if motile sperm persist |
| British Andrology Society | 16 weeks & after ≥24 ejaculations | Two consecutive sperm-free samples | Additional testing, continued contraception |
| American Urological Assoc. | 8–16 weeks post-vasectomy | Azoospermia or rare non-motile sperm | Counseling, possible repeat procedure |
Frequently Asked Questions
What is the purpose of post-vasectomy semen testing?
Post-vasectomy semen testing confirms the effectiveness of the procedure by ensuring there is no presence of sperm in the ejaculate, allowing men to stop using alternative contraception.
How long after a vasectomy should I get a semen analysis?
It’s recommended to perform a semen analysis 8 to 16 weeks after the vasectomy to allow enough time for residual sperm to clear from the reproductive tract.
What guidelines should I follow for semen sample collection?
You should abstain from ejaculation for 48 hours to 7 days before collection, collect the entire ejaculate into a sterile container, and ensure the sample is delivered to the lab within one hour for accurate analysis.
What if my semen analysis shows the presence of sperm after a vasectomy?
If motile sperm or more than 100,000 non-motile sperm are detected, it may be necessary to repeat the test and consider further consultation with your healthcare provider regarding potential next steps, which could include a repeat vasectomy.
Recommended
- Why Test Semen Sample: Answers for Vasectomy & Fertility 2025
- Why Semen Testing Is Critical: Insights for Men and Clinics
- Semen Test Kit Instructions for At-Home Vasectomy Confirmation 2025
- Patient Adherence Post Vasectomy: Key Steps for Success
- Post Vasectomy Semen Test Timing - Understanding When
- Home Testing vs Clinical Testing for Vasectomy Confirmation 2025





